Musculoskeletal conditions: Part one - a primer

Musculoskeletal disorders (MSDs) are a leading cause of compensated injury – but what exactly are we referring to when we talk about the musculoskeletal system? Here’s a brief rundown, modified from Wikipedia:
The musculoskeletal system is the system that gives people the ability to move using the muscular and skeletal systems.
It is made up of the body's bones (skeletal system), muscles, cartilage, tendons, ligaments, joints, and other connective tissue that supports and binds tissues and organs together.
Bones are connected to other bones and muscle fibres via connective tissue such as tendons and ligaments. The bones provide the stability to a body, like iron rods in concrete construction. Muscles keep bones in place and play a role in movement of the bones.
To allow motion, different bones are connected by joints. Cartilage prevents the bone ends from rubbing directly on to each other. Muscles contract (bunch up) to move the bone attached at the joint.
When things go wrong
Problems arising from the musculoskeletal system are common in the community. Studies of populations of people tell us that over 50% of adults have long term soreness arising from a component of their musculoskeletal system. Examples of this include:
- A long term backache that is more troublesome from time to time;
- A shoulder soreness that flares with overhead activity; and/or
- Long term generalised ache in the arms that the person recognises is sorer when they become stressed.
The types of musculoskeletal conditions that are now common are different from those that were common a few decades ago. Changes in workplace technology have led to an increase in musculoskeletal disorders, as workers use different equipment and different motions. For instance, the overuse of personal digital devices has led to sprained thumbs becoming more common.
Many people live with their soreness; some seek health care if the pain worsens. Other times people attend their doctor or physiotherapist when they are concerned, wanting to make sure they do not have a serious condition that needs treatment.
Whilst medical care can do a great deal for a number of health problems, treatment for musculoskeletal problems provides only limited benefit.
Some common facts about MSDs
- Over 50% of the population has a long term musculoskeletal complaint.
- In 2004–05, 31% (6 million) of the population (33% of females and 29% of males) reported having a long-term diagnosed disease of the musculoskeletal system and connective tissue.
- In the National Health Survey of 2004–05, musculoskeletal conditions were the most commonly reported long-term condition due to an injury. Musculoskeletal conditions accounted for a quarter (25%) of all long-term conditions. Of those reporting musculoskeletal problems:
- 31% had back problems;
- 16% had ‘rheumatism’ and other soft tissue disorders; and
- 12% of those with arthritis reported the condition was due to an injury (ABS 2006c).
- Back, neck, shoulder, arm and knee problems are the most common musculoskeletal conditions.
- Most problems are mild and bothersome, rather than interfering with all activities.
- The pain from a musculoskeletal condition can be severe, e.g. back pain: where there is muscle spasm present, or in the early stages of an injury.
- Musculoskeletal conditions can get better quickly, i.e. in a few days, or can take a long time to settle. For example: 25% of new episodes of back pain can take up to 2 years to settle.
- Most people with musculoskeletal conditions can return to a good level of function within days to weeks, depending on the condition and the treatment approach.
- In any one year, 10 per cent of the community advises they have had an episode of back pain severe enough to significantly limit their activities.
- About one in six people in the community has a long term back problem, aching most of the time and causing more substantial pain perhaps a few times each year.
Management of musculoskeletal injuries
The management of musculoskeletal conditions varies between practitioners. Here, we use the example of back pain to illustrate the general approach taken in managing musculoskeletal problems.
While the approach that medical practitioners take towards patients with back pain injury can vary substantially, the diagram below illustrates five basic treatment principles practitioners are encouraged to follow:
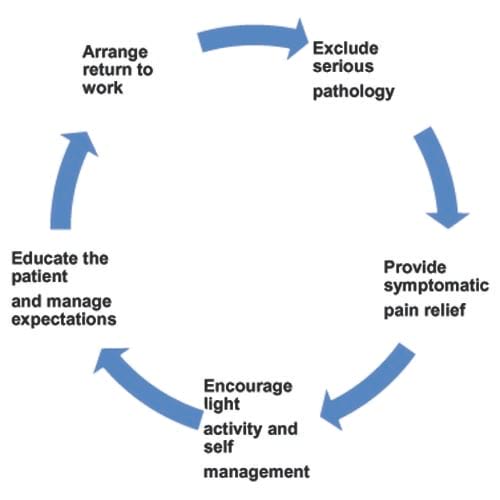
An explanation of each of these principles is shown below:
|
Principle |
Description |
|
Exclude serious pathology |
Ensure a thorough history of the patient is taken and a full examination made. Pay particular attention to how the injury occurred. Eliminate conditions such as fractures, spinal cord and nerve root compression etc. |
|
Provide symptomatic pain relief |
Determine the most effective pain relief treatment applicable for the patient. This may involve prescribing analgesic medication, or referral to physiotherapist etc. |
|
Encourage activity and self management |
Encourage the patient to stay active and live as normally as possible, as this improves the rate of recovery and reduces work absence. |
|
Educate the patient and manage expectations |
Communicate effectively with the patient to avoid the development of fear avoidance beliefs, i.e. anxiety, which can prolong disability and recovery. Educate the patient in why an early return to work is beneficial and that normal behaviour is unlikely to cause further harm. |
|
Arrange return to work |
Communicate to all parties concerned the medical restrictions, likely prognosis and graded return to work based upon the expected natural progress of the condition (rather than reported pain levels). Monitor the patient’s progress on a regular basis. Ensure that the medical certificate states clearly what is and isn’t permitted in terms of physical restrictions, alternative duties and hours of work. |
Unfortunately, this approach is not always followed. Many factors influence the treating practitioners approach:
- Are they up to date with best practice and evidence based medicine?
- What does the patient want? Doctors tend to want to care for their patient, and will often be influenced by what they perceive the patient wants in terms of treatment and returning to work.
- Is the patient distressed? Distressed patients influence how doctors treat their condition. Distressed patients have more investigations and treatment (they press their doctors with their concerns, leading to more tests and treatment being done). This is a problem when extra medical care causes more harm than good.
The following table illustrates the comparison between a traditional and a modern approach of practitioners towards workers who are suffering from a back injury:
|
Traditional biomedical education |
Modern biopsychosocial information and advice |
|
Focus on relieving pain. |
Focus on improving function. |
|
Provide a diagnosis, e.g. tell the patient their scan shows they have a disc problem. |
Provide practical advice on how to manage their condition. |
|
Provide medical information about anatomy, pathology, diagnosis, and treatment. |
Provide information about the usual course of the condition, and how they can best manage their condition. |
|
A series of restrictions are provided, i.e. the patient is told what they can’t do. |
Focus on staying active, continuing ordinary activities as normally as possible and activities of daily living. |
|
Facilitate patient cooperation with treatment. Patient remains the passive recipient of professional treatment. |
Enable individual to share or take over responsibility for his or her own continued management. |

